© Ken Sinervo MD, MSc, FRCSC. All rights reserved. No reproduction permitted without written permission. Revised since original publication and current as of 2023. No external funding was utilized in the creation of this material. The Center for Endometriosis Care neither endorses nor has affiliation with any resources cited herein. The following material is for informational purposes only and does not constitute medical advice.
ADHESIONS: AN UPDATE
© Ken Sinervo, MD, FRCSC, ACGE, Medical Director
This is my third update on adhesions since joining the practice in 2001. Over those years, we have tried several products indicated for adhesion prevention and used others that have additional benefits for healing and adhesion prevention. These efforts remain a continuing process of perfecting our surgical techniques and therapies to maximize outcomes, including adhesion prevention and reducing endometriosis recurrence.
The incidence of adhesion formation depends on many factors. Patients with advanced stages of endometriosis (stage III and IV) often have a significant amount of adhesions prior to any surgery, because endometriosis itself can cause adhesions to form. The amount of raw peritoneal surfaces left following excision surgery may help us anticipate the likelihood of adhesion formation. The use of adhesion barriers often helps to reduce this risk.
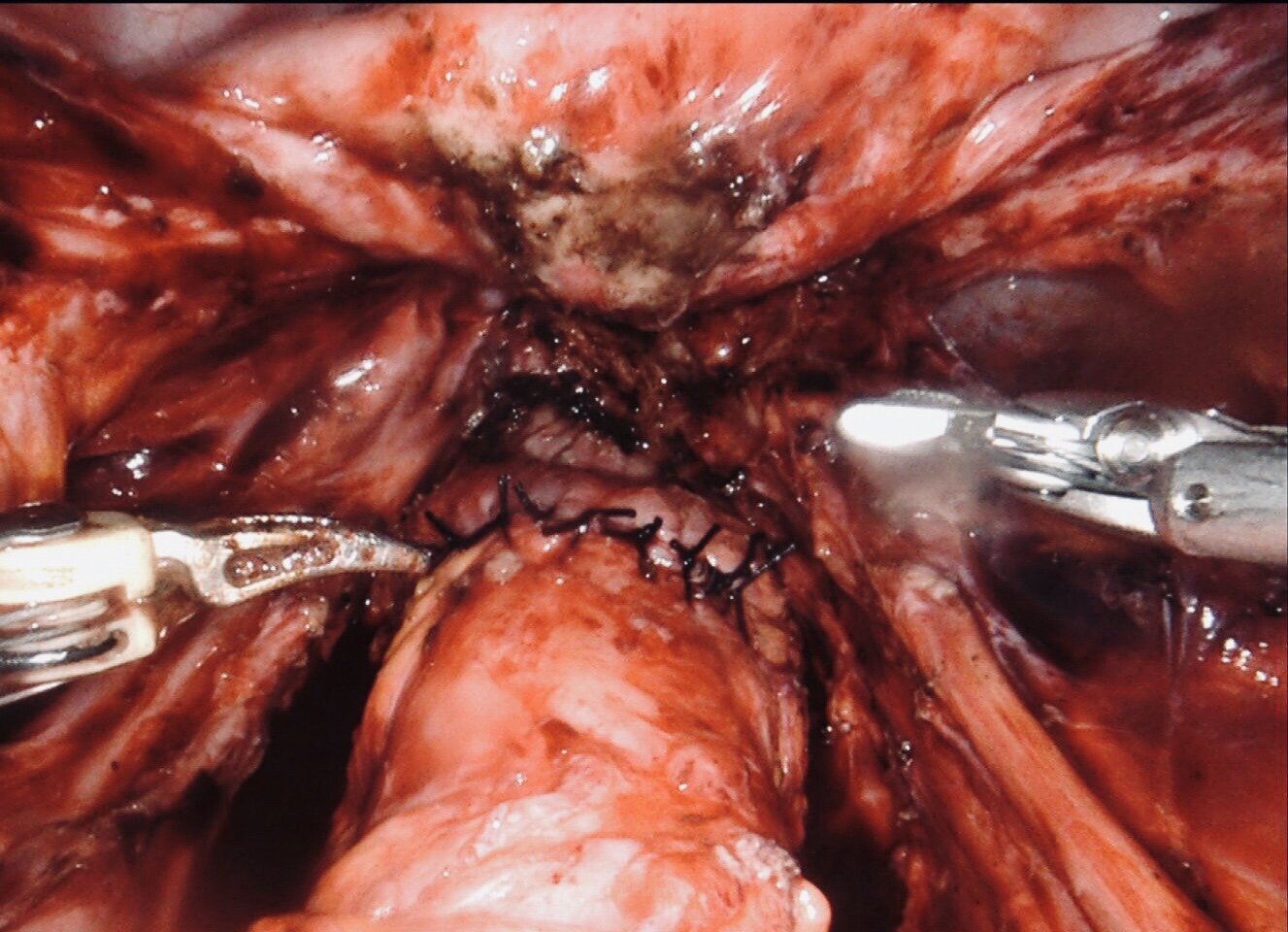
From left: dense adhesions in a patient who had been on hormone suppression for years; no prior lysis (removal) or excision performed. The middle image is immediately following lysis and meticulous excision of all endometriosis. The final image (far right) is at the time of a later procedure, which revealed healthy tissue, mobile structures and no recurrent disease. Images © Dr Jeff Arrington
There remains no substitute for excellent surgical technique. Adhesions can be separated sharply or bluntly; however, an approach that minimizes tissue injury and excessive use of cautery is preferable. This includes minimizing injury to tissues through the careful use of atraumatic instruments that do not crush tissue or leave denuded surfaces. Preventing blood loss is important, as intra-abdominal blood can increase the chances of adhesion formation. When bleeding cannot be prevented, bipolar cautery is used to control it. Copious irrigation helps to remove any remaining intra-abdominal blood. Finally, the judicious of carefully selected sutures may help prevent foreign body reactions.
Products
A number of products have been used to help minimize the formation of adhesions. Barrier agents include non-absorbable barriers, absorbable barriers and fluids. These agents prevent adhesions by physically separating damaged tissues during peritoneal healing, the time during which adhesions form. This healing period is usually considered to be a few days to a few weeks.
Non-Absorbable Barriers
Non-absorbable agents include Gore-Tex and Shelhigh No-React. These agents were initially used during heart surgery. They must be sutured into place, and because they do not dissolve, must theoretically be removed at a later date to prevent fistula formation. The need for a second surgery has limited their widespread use in gyn surgery. I have rarely used Gore-Tex in patients requesting it and have not seen any significant improvement over our current regimen, and it does expose the patient to another surgical procedure and its inherent costs and potential complications.
Absorbable Barriers
There are several absorbable barriers that have been used over the years. Some have come and gone. The only one that has been shown to have any benefit is a product called Interceed. It is derived from oxidized regenerated methylcellulose. It looks like a fine silky mesh that can be cut and laid over top of the injured tissues or areas that we are trying to prevent tissue re-adhesion (usually the ovaries, uterus and bowel occasionally. Within eight hours, it becomes a gelatinous protective layer that is absorbed within 2 weeks. It separates the tissues, allowing them to heal individually during the time of vulnerable adhesion formation. It does not need to be sutured in place, which is good since absorbable suture can increase the risk of adhesion formation as they cause inflammation and take a long time to dissolve. Numerous studies have demonstrated a reduction in adhesion formation. It has an extremely good safety profile, with no reported allergic reactions. Having meticulous hemostasis is necessary, since the presence of blood may increase the risk or scarring and adhesions.
Seprafilm is a bio-absorbable membrane derived from sodium hyaluronate and carboxymethylcellulose. Within 24 hours of placement, the film becomes a hydrated gel that is absorbed by the body within seven days. Initial studies demonstrated optimistic results. Because of the difficulty in using the stiff sheets, some doctors began creating a slurry in which several sheets were cut up and mixed with normal saline. This was then sprayed or applied to cover the surfaces where adhesions may form. Unfortunately, studies in Europe demonstrated increasing complications following its use, and ultimately a ban on its use as a slurry. Similarly, there have been serious complications in the US as well, and it is rarely used here anymore. See https://www.justice.gov/opa/pr/genzyme-corporation-pay-325-million-resolve-criminal-liability-relating-seprafilm for additional information. It is still available as a sheet that should not be altered, and likely will only be used in open surgery or laparotomy.
Coseal and Tisseel are products that have been advocated for use in prevention of adhesions. These are products that indicated for use in vascular surgery to reinforce a graft to help with hemostasis. It should not be used for adhesion prevention. Similarly, Tisseel has been used for hemostasis when traditional options have failed and for use to reinforce the site of a bowel resection. There are some small studies that have suggested benefit but these are not approved by the FDA for adhesion prevention. It can be used as an off-label use, but my experience has shown that when used in the pelvis, these products result in more adhesions. Similarly, Arista, a product intended for use for hemostasis has also been suggested for off label use for adhesion prevention. It is made up of microporous polysaccharide spheres (Arista) that form a polysaccharide powder made from potato starch. It absorbs water, concentrating platelets and other proteins to accelerate clot formation. In the patients that we have seen it used in, we have also seen increased adhesion formation above what we would expect to be normal after the described surgery, so we do not recommend its use, either.
Fluids
Absorbable fluid adjuvants have many advantages to barrier agents such as Interceed and Seprafilm because they coat all surfaces, whereas barrier agents are placed over areas considered to be most likely to form adhesions. Intergel, an 0.5% form of ferric-coated hyaluronic acid (hyaluronic acid is a component of body tissues and fluids such as peritoneal fluid), was shown in a number of studies to reduce the risk of adhesion formation by 40-50%. Unfortunately, Intergel was withdrawn from the market following reports of adverse reactions including post-operative pain, possible foreign-body reaction and adhesion formation.
Spraygel is a product that is currently in clinical trials in the United States. Two polyethylene glycol (PEG)-based liquids are mixed during spraying and form an adherent absorbable hydrogel. It adheres to the tissues that it is sprayed to and remains intact for 5-7 days, the critical period of healing, and then degrades into an absorbable and easily excreted by-product. The frequency and amount of adhesions were decreased in initial studies by about 70%. It has been almost 10 years since initial clinical trial were undertaken in the United States, and FDA approval is still pending. It is unlikely that it will be approved at any time soon.
Adept is a 4% icodextrin solution that can be placed at the end of the surgery to help reduce adhesions. It takes several days to be absorbed and acts as a hydro-flotation to separate tissues while healing. The benefits seen in clinical trials were small, and post launch surveillance studies demonstrated a fairly high rate of complications. It should also not be used in laparotomy, or surgeries in which bowel resection have been performed. With the minimal benefits, and relatively higher complication rates, we do not use this product anymore.
PRP, or Platelet Rich Plasma is a product derived from the blood of the patient undergoing surgery. Plasma is the blood product that is left over after the red blood cells have been removed. This is further concentrated to form platelet poor and platelet rich plasma. We take the platelet rich plasma, and spray or inject it onto the raw surfaces that are present after excision of endometriosis and adhesions. A study in 2007 demonstrated reduced pain following laparoscopic surgery with the use of PRP. Initial use of it in our practice demonstrated this as well. One of the additional benefits that we saw was a reduction of adhesion formation in the patients that we operated on. We saw a reduction of surgeries needed for adhesion induced pain, and also, when we re-operated on patients for any reason, we saw that those that had PRP used, had a reduction in adhesion formation compared to those who had not received it. This makes sense because PRP has been used years in several other areas of medicine to help with healing such as orthopedics, plastic surgery, ophthalmology, and orthodontics are just a few. The mechanism of action likely has to do with the presence of growth factors within the PRP and this promotes healing, and through faster healing, we have less chronic inflammation and adhesion formation. We have used it in close to 2,000 patients since 2013 with excellent results.
Finally, Amniotic membrane is another product that has been used in several studies to reduce adhesion formation and improve healing. There are numerous studies demonstrating its effects on healing. I personally saw its actions when I had it injected into a non-healing partially torn Achilles tendon where the tendon joins the calf muscle. After 8 weeks of persistent pain, I had the tendon injected and within 3 days, my pain resolved and it has remained pain free for over 5 years. Additionally, my brother was recovering from a cancer surgery where a full thickness skin graft was used, and the in area that was taken from, the partial thickness skin graft used to repair the full thickness graft site stopped healing. No healing occurred despite the plastic surgeon using every option available to him. I suggested my brother use the amniotic membrane with the approval of his plastic surgeon, and within 3 weeks, the donor site was fully healed. This is one of the reasons that it is used in diabetic wounds/ulcers when other treatments have failed. Animal studies demonstrated reduction in adhesions. Additional studies demonstrated benefit in other surgeries such as urologic and spine surgery, with reduction of adhesions. We have been using it for over 4 years with excellent results in patients with severe disease. It also has demonstrated a reduction in adhesion formation in our second look surgeries performed for recurrent pain (usually due to adenomyosis and not necessarily endometriosis recurrence or adhesions).
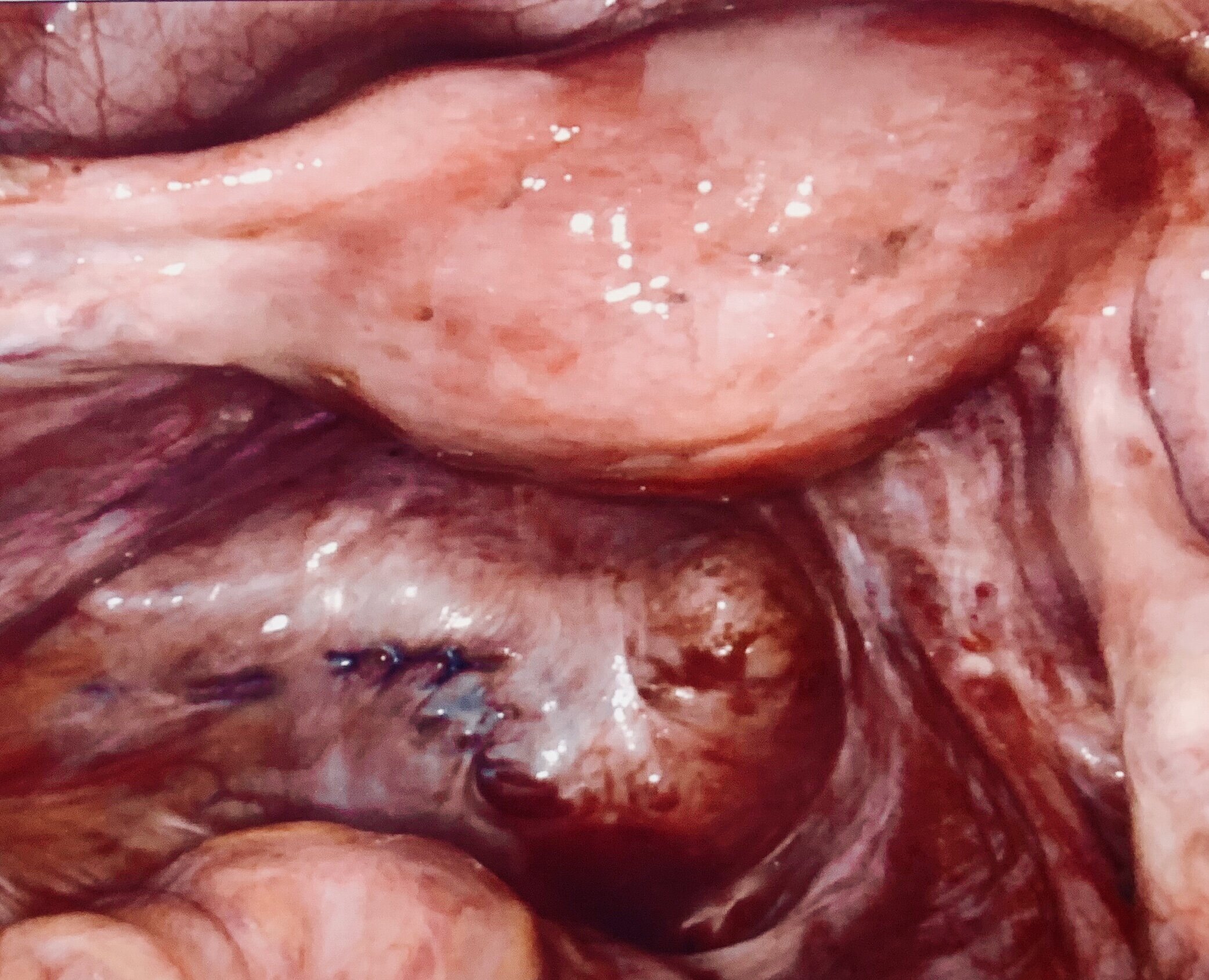
Ovarian Suspension
Finally, since our last update, we have also been performing ovarian suspension in patients that have had endometriomas or severe endometriosis with extensive adhesions being present as well as extensive deep excision along the pelvic side walls and posterior cul de sac area, where the ovaries are more at risk of adhesion formation. There are several studies demonstrating the effectiveness of ovarian suspension in the prevention of adhesions following advanced gynecologic surgery, including endometriosis excision:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3119028/
https://www.ncbi.nlm.nih.gov/pubmed/30092363
https://link.springer.com/article/10.1007/s10397-016-0963-3
We have been performing ovarian suspensions for several years now and have excellent results with this technique. It does necessitate the removal of the non-absorbable suture after about a week, but can easily be done in the office or even at home. Watch: https://www.youtube.com/watch?feature=youtu.be&v=ZgHaBUfTtp4
Conclusion
In conclusion, the most important factor to prevent the formation of new adhesions, and recurrence of previous adhesions, are the surgical techniques used by the surgeon. Minimizing bleeding initially, using tissue sensitive techniques, avoiding unnecessary cautery, following the natural tissue planes, and in my opinion, the tissue sparing and low impact effect of the laser on the tissue that does not devascularize the surrounding tissues, are all important to help reduce scarring or adhesions. Use of adjuvant techniques, such as Interceed, PRP, amniotic membranes and ovarian suspension has greatly reduced the need for future adhesion surgery, especially in severe cases of endometriosis. In those patients that do develop clinically relevant recurrent adhesions – those with symptoms due to the adhesions (less than 5% of our patients), if surgery is needed, and there is little or no endometriosis present which is also the case in well over 90% of our patients, the likelihood of recurrent adhesions becomes even less.
Click here to read more educational articles and information in our Endo Library